I remember studying male and female reproductive medicine in my medical science class during the last school year. I flipped through the vocabulary terms for the men’s section, and when I went to the women’s section, I noticed that the amount of things that could go wrong with a woman’s body was significantly greater than that of a man’s. At first, I saw it was because of how many sections there were — problems to do with the menstrual cycle, pregnancy, the postpartum period, lactating, menopause, and in general, any malfunctions or diseases of all of the parts of a woman’s anatomy itself. This got me thinking about how many more processes the average woman must go through in her life compared to a man, and how these are all opportunities for health issues to arise. And, unfortunately, there are disparities between the way women’s and men’s health are treated.
For example: the stigma.
“Stigma is experienced across many women’s health services by both patients and health providers around the world,” the Royal College of Obstetricians and Gynecologists states. “The stigma that surrounds women’s health conditions and procedures leads to them frequently being deprioritised [sic] within health budgets and services.”
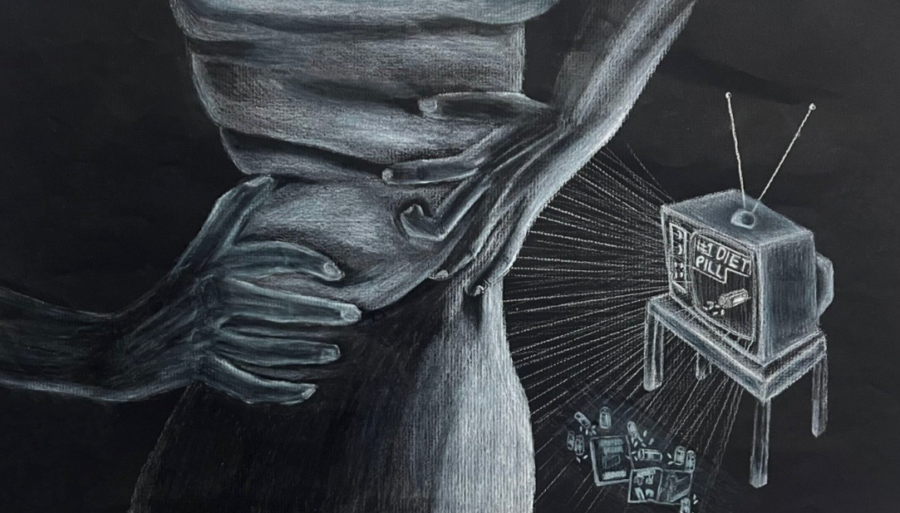
Women are neglected when it comes to their health. Forbes states that women are unfairly reflected in healthcare research, which means that there are fewer treatments available for female-specific diseases.
“Women’s bodies function differently than men’s,” Forbes states. “There are obvious reproductive differences that impact women throughout their life—fertility and pregnancy issues, menopause as well as other gynecological disorders and cancers of the breast, ovaries and cervix that affect women.”
The treatment that can be accessed for these multitudes of conditions is incredibly expensive, since a woman’s body is scientifically a lot more susceptible to a lot more problems. WebMD reports that in terms of out-of-pocket health care expenses, working women pay as much as $15.4 billion more per year than men.
Women’s health has also been considered a hassle, as women must make regular trips to the gynecologist and deal with endless political arguments over their rights to their bodies.
“In post-Roe America, many women seeking abortions are treading on landmines, particularly in states where access is banned or severely restricted,” The Commonwealth Fund says.
Guttmacher Institute discusses the Hyde Amendment, which was placed into effect in 1977. It essentially bans federal dollars from being used for abortion coverage for women insured by Medicaid, which is the nation’s main public health insurance program for low-income Americans.
“Women who are low-income and lack insurance coverage for abortion often struggle to come up with the money to pay for the procedure,” Guttmacher says. “As a result, they often experience delays obtaining an abortion or are forced to carry their unintended pregnancy to term. Supporters of abortion rights have coalesced behind several state- and national-level initiatives that aim to end the Hyde Amendment, so that the nation’s poorest women have greater access to safe and legal abortion care.”
Though women have certainly come a long way in earning their deserved rights, stigmas unfortunately still linger.
“Discussions of menstruation have continued to reinforce shame around the issue through the 20th and 21st centuries, portraying periods as something to be embarrassed about and to be kept hidden,” the Conversation says.
Personally, a lot of the time it feels like it isn’t right to talk about menstruation out loud, as if it is something to conceal and something that feels wrong or that other people shouldn’t have to be exposed to.
A survey by the girls’ rights charity “Plan International UK” revealed that “the shame and silence around periods is stopping girls from seeking medical advice for menstrual symptoms they are concerned about” — 79% of girls and young women have experienced symptoms linked to their period that concerned them, but haven’t seen a doctor or health professional.
Endometriosis UK states that 62% of women (aged 16-54) would put off going to a doctor with symptoms of endometriosis because they “don’t think it’s serious enough to bother a doctor with, they’d be embarrassed, don’t think they’d be taken seriously, or think symptoms including painful periods are normal… this statistic rises to 80% of 16-24-year-olds.”
Stigmas such as these are harmful towards women’s health, as they keep women quiet about problems that they should have no problem getting treated and taken care of. These stigmas can also contribute to feelings of inadequacy, or feelings that these health problems aren’t crucial enough to be taken seriously, and can also be detrimental to women not getting the care that they need. Another unfortunate statistic shows that 47% of the female population (aged 16-54) would be concerned to tell their employer they needed to take time off sick due to endometriosis, rising to 57% of 16-34-year-olds.
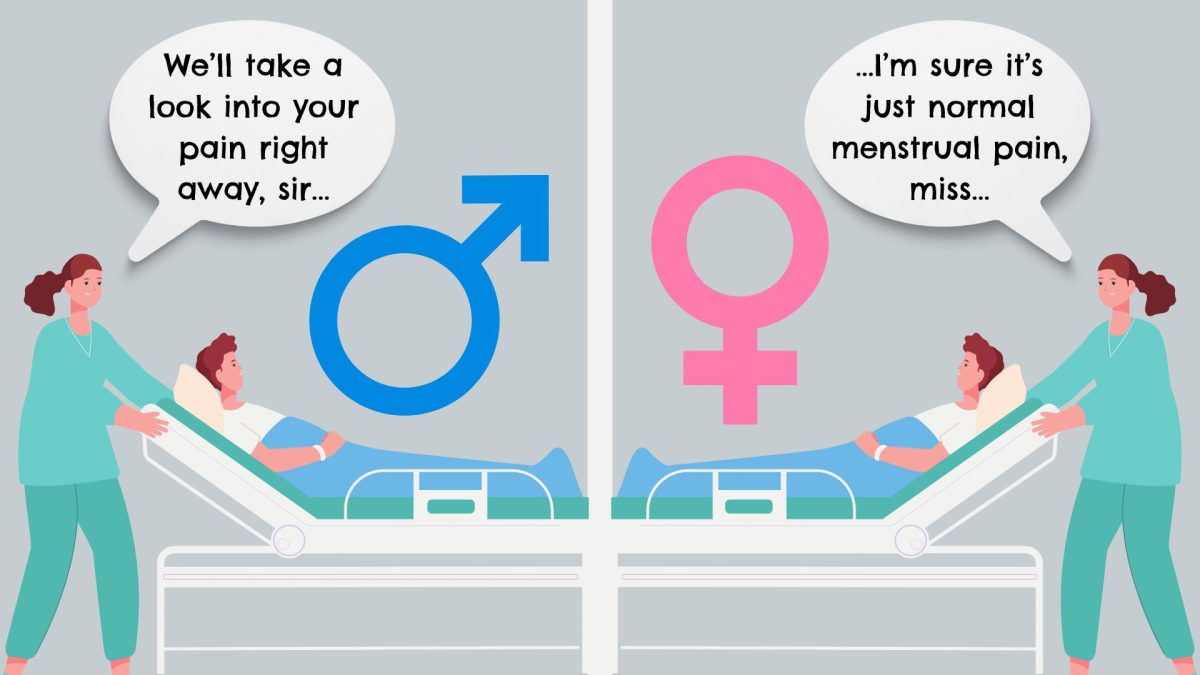
The dangerous attitude of underestimating women’s complaints about their health and well-being has contributed to detrimental health impairments for the female sex.
The Washington Post discusses these disparities, recounting anecdotes about how one woman was told she was being “dramatic” when asking for a brain scan after months of suffering headaches, and it turned out that she had a brain tumor; another was ignored while in pain during a 33-hour labor, the fact that her epidural fell out going unnoticed; and dozens of women complained of torturous pain as their vaginal walls were punctured during an egg retrieval process, whom were then told that their pain was normal and received saline instead of anesthesia.
“A number of studies support the claim that women in pain often are not taken as seriously as men,” the Washington Post says. “This year, the Journal of the American Heart Association reported that women who visited emergency departments with chest pain waited 29 percent longer than men to be evaluated for possible heart attacks.”
Women are thought to have higher pain tolerances than men, since they go through more biological processes throughout their lives, such as menstruation, pregnancy, and menopause, to name a few. This belief, however, can be unfair toward women.
“An analysis of 981 emergency room visits showed that women with acute abdominal pain were up to 25 percent less likely than their male counterparts to be treated with powerful opioid painkillers,” Washington Post says.
Additionally, many women are put through painful procedures, such as IUD insertions, without sedation, as it is believed that if a woman can go through childbirth or is used to menstrual cramps, pain in those regions is nothing new to her.
Healthline says, “For many people, the insertion process is more uncomfortable than painful…others experience moderate to severe pain during the process, including intense cramping and pressure on the abdomen. You might also break out into a sweat, feel nauseous or vomit, or, in some cases, faint.”
This list casually ends with: “These side effects generally subside over the next few hours or within the next day.”
Are women expected to accept these side effects as normal? Would men be treated so lightly in terms of their side effects if they were described like this?
If men want easy and reversible birth control, they only need to have a vasectomy — an outpatient procedure much easier in comparison to a woman tying her tubes, a much more invasive procedure that involves cutting the fallopian tubes. There aren’t a million options with a million side effects offered to men — it’s just a lot simpler for them.
Contraception methods are just one example of women struggling more in terms of their physical well-being than men. Besides birth control, penetration, menstruation, pregnancy, childbirth, and postpartum recovery are all very painful to deal with — and just because these processes are something that we are expected to go through during our lives does not mean that our health shouldn’t be taken seriously or taken care of in the same way it would be if a man complained about it.
If there are pages and pages more of things that could go wrong with a woman’s body in comparison to a man’s, it seems logical that more focus should be directed to female health. However, the status quo reflects the opposite. Closing the gap between these disparities concerning sex and gender is essential to providing women with the care that they deserve.